UK healthtech pioneer, my mhealth and collaborators awarded €2.5M Eurostars Grant for better heart health project.
Immersive cardiac rehabilitation app, myHeart uses behavioural feedback and gamification features to improve patient well-being.

NHS-approved digital therapeutics company, my mhealth, with 3 European collaborators, have been awarded a highly prestigious €2.5M Eurostars Grant for the development of their innovative project, CUOREMA. Eurostars is a European joint programme, co-funded from the national budgets of 36 EUREKA countries and by the European Union through Horizon 2020. As a UK funding body, Innovate UK will sponsor my mhealth Limited to develop part of its myHeart app to support cardiac rehabilitation in Europe.
Together with three accomplished European partners; Ospedale Malcantonese (OSCAM) (Switzerland), Games for Health (The Netherlands) and the University of Applied Sciences and Arts of Southern Switzerland (SUPSI) (Switzerland), the project aims to utilise the cardiac rehabilitation element of the myHeart app and incorporate biofeedback, intelligent algorithms and gamification features. During the three years of planning and development, the platform will be formally researched in the UK and several European countries through formal clinical trials.
The CUOREMA project will focus on developing a new, patient-centred and intelligent cardiac rehabilitation support system. The scalable, customisable, and flexible technology will provide a new systematic method of social and biological feedback from wearable devices, the app will include built-in behaviour change support systems, with mixed reality and immersive technology to improve medical adherence and clinical outcomes.
The Eurostars Programme is a funding and support programme, aimed at R&D-performing SMEs that wish to redeem the benefits that come with international collaboration. The application process is hugely competitive, with 506 applications submitted from across 36 countries. The evaluation process considers three key areas for assessment; Quality, Impact and Excellence.
As the project lead, my mhealth are clinical and technological experts in digital healthcare applications for long-term conditions, with COPD as a primary area of focus. Their expertise in this arena, and vision and experience in digital therapeutics was recognised by the judging panel. In particular the project achieved the highest scores in the Innovation & R&D category.
In following strict guidelines the app will be compatible for use across the European Union, once developed the app content will be available in five languages: French, Italian, Portuguese, German and Spanish.
Dr. Simon Bourne, Chief Executive Officer of my mhealth:
“We are thrilled to be partnering with such talented and diverse teams on this innovative and important project over the next few years. Each organisation brings a very unique perspective to the table, allowing for a thoughtful and comprehensive approach to tackling heart health. I am extremely passionate about digital health and this has the potential to change many lives for the better, helping us transform cardiac rehabilitation for patients across Europe.”
About my mhealth:
Our mission is to change healthcare forever. We do this by empowering patients and clinical teams to manage long-term conditions using digital therapeutics, delivered remotely at a fraction of the traditional cost to patients with Asthma, COPD, COVID-19, Diabetes and Heart Disease.
Founded by two NHS medical consultants to deliver evidence-based interventions using software and applications to patients, we developed the UK’s first NHS-approved digital platform. My mhealth delivered over 275,000 rehabilitation and education sessions during 2020 to patients with respiratory and cardiac conditions.
Each of our apps, including myCOPD, myAsthma, myDiabetes and myHeart, have been developed with clinical experts in their field to provide patients with the knowledge and support to manage their conditions. These self-management apps offer a unique, customised, and personalised experience for patients and they can be accessed and used on almost any device, from smartphones to smart TV’s.
We are pioneering a new approach to dispersed healthcare provision, enabling remote monitoring, and medication management which delivers better outcomes, improved patient engagement and decreases the burden on the NHS.
About Games for Health:
Games for Health is a research & design driven SME, based in the Netherlands with over 20 years’ experience application design based on playful intelligence for healthcare and other markets. Playful intelligence allows for a desired change in behaviour among individuals, as well as larger groups as it calls on the natural youthfulness of our desire to play. Being a specialist in this field, Games for Health has designed many applications for therapy adherence, anti-biotics prescriptions in the struggle to overcome anti-biotic resistance and lifestyle change in case of infertility problems for several leading pharmaceutical companies. In several European consortia it works on motivational strategies, e.g. for stress relief of elderly employees (mHealthINX), for the stimulation of physical activities in the younger population (Sugapas) and also on planetary health related topics like environmental influence on cardiopulmonary diseases (Expanse) and reversed logistics of e-waste. It’s most recent success is the Post-IC digital diary for the prevention or relief of the post intensive care syndrome, of major importance in times of Covid-19 (Post-icu.com).
About Ospedale Malcantonese (OSCAM):
The Ospedale Malcantonese is a non-profit organisation, established in 1928 thanks to the donation of Mr. Giuseppe Rossi of Castelrotto, officially inaugurated on 11 November 1928. The Ospedale Malcantonese is included in the hospital planning of the Canton Ticino (Switzerland).
The Ospedale Malcantonese has a RAMI department (Acute Department of Minor Intensity), a psychiatry department and various outpatient services (Cardiology, Cardiovascular Prevention and Rehabilitation, Physiotherapy, Ergotherapy, Dietician, Radiology, First Aid, Psychology, Diabetology, Advice for smoke sessecion, Laboratory Analysis, Acupuncture, Abdominal and Vascular Ultrasound, Pulmonology, Social Assistance).
The Ospedale Malcantonese is represented by Dr. Tania Odello (Senior Cardiologist of the Cardiology Service and of the Rehabilitation and Preventive Cardiology Service) and the CUOREMA Cardiovascular Rehabilitation Team, from which the name of the project originates from (www.cuorema.com). They will specialise in the clinical development of the CUOREMA App, the clinical study that will support the project and ethical supervision.
About the University of Applied Sciences and Arts of Southern Switzerland (SUPSI):
Dr. Francesca D. Faraci is the leader of the Bio-Signal Processing (BSP) research group of the University of Applied Sciences and Arts of Southern Switzerland (SUPSI) Department of Innovative Technologies (DTI). The research focuses on the optimisation and tailoring of advanced statistical and AI methods, to individualise clinical medicine for monitoring, diagnostic and therapeutic applications.
In the European project CUOREMA, SUPSI-DTI-BSP will be in charge of developing the bio-behavioural change support system. BSP researchers will build upon objective, subjective and contextual information about the patients; interpret the information considering the clinical and social individual characteristics and feed this information back into the system to enhance the adherence to CVR, also through gamification. Our biggest challenge is to develop algorithms that integrate different perspectives, ensuring clinical, social, psychological, technical, gamification and computational needs are taken into account.
ALFAGAMMA and L.I.F.E. sponsors
The project will benefit from the collaboration and support of the company ALFAGAMMA (www.alfagamma.ch), distributor and manufacturer of medical devices and with the company L.I.F.E. (www.x10y.com), manufacturer of advanced intelligent garments that will allow us to monitor our patients in an innovative way, even from a distance.
If you want to find out more about this project or how myHeart can help your cardiac patients please get in touch here or call us on +44 (0)1202 299 583.
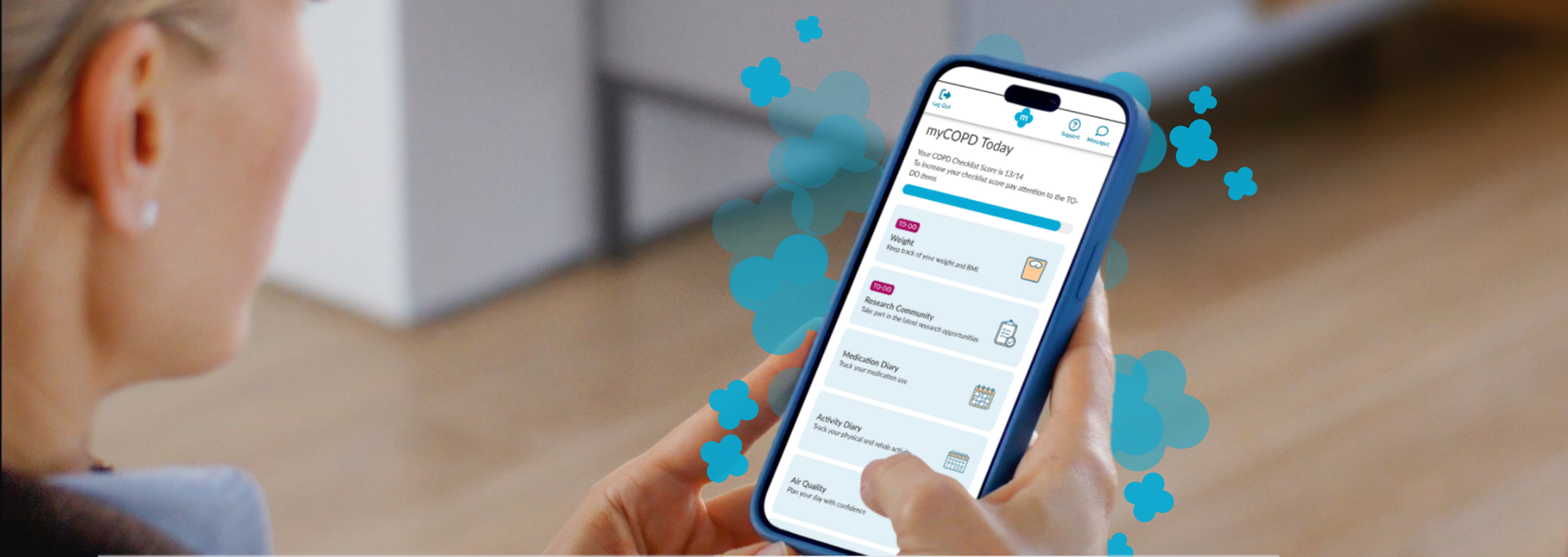
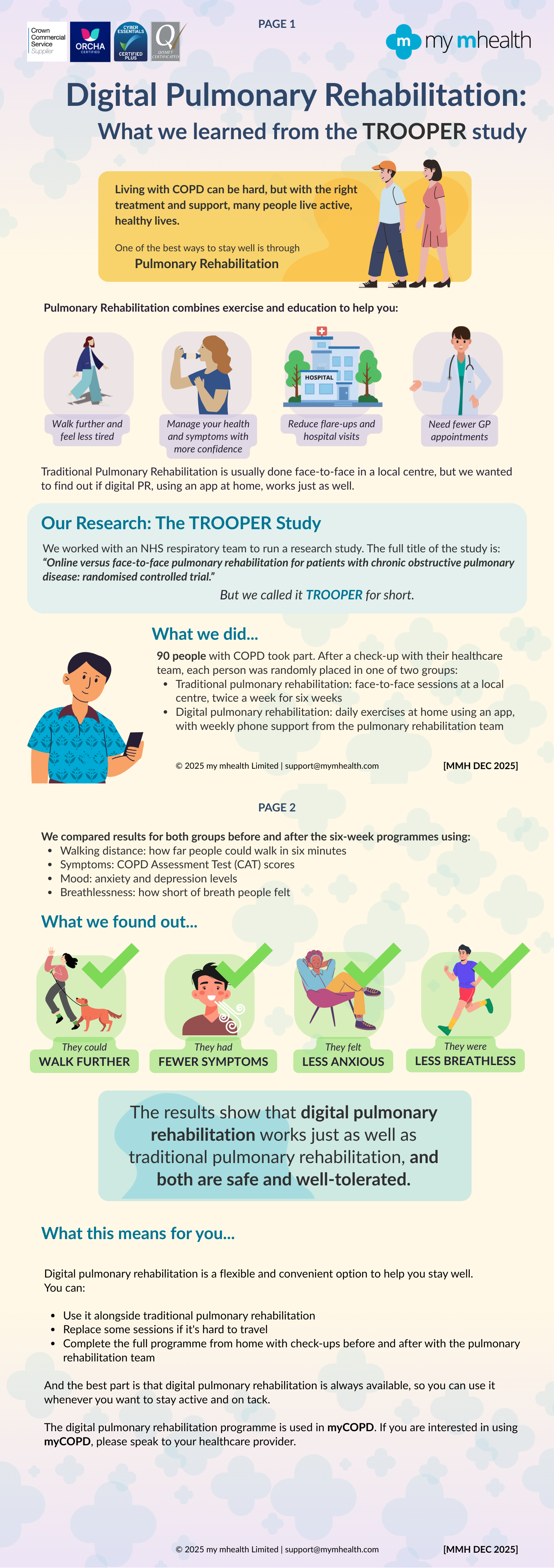
Your Feedback, Our Improvements We want to make sure our product is designed with your needs in mind. To achieve this, we regularly send out surveys and work closely with our Patient & Public Involvement (PPI) group, ensuring that your feedback directly shapes improvements and updates. We received 147 responses to our Research Community Survey .. said they found our app easy to use Overall, most of you said you had positive experiences of using the app .. said you would keep using it to manage your condition Our PPI activities have helped us to make important changes... Navigating around isn’t always that easy The home screen menu is now grouped into smaller sections with a ‘To Do’ list to help you stay on track Too many questions at the start makes it just too complicated Most of the questions at the start have now been removed so you can get started sooner We have now expanded the nutrition information which also contains a nutrition questionnaire to provide you with personalised advice There is not enough information on nutrition. Sometimes I forget to eat What we are working on We are creating a ‘Prepare for Your Appointment’ function in myCOPD and myAsthma We are planning to include a ‘Search’ function so you can get to what you need quickly Keep talking to us! Your experiences help us continue to improve.If you would like to share your thoughts or be part of our Patient and Public Involvement group, please join the Research Community. We would love to hear from you

A new partnership between leading digital health innovators, my mhealth and Patients Know Best (PKB) means shared NHS customers can streamline the delivery of their digital care tools, making it easier to empower patients to manage their health effectively. The collaboration brings together my mhealth’s award-winning self-management platforms with PKB’s personal health record solution, which is already embedded within the NHS App. “At the heart of this partnership is the patient,” said Dr. David Pettigrew, CEO of my mhealth . “By aligning our platforms, we’re enabling people to take greater control of their health while supporting clinicians with joined-up, efficient care pathways. It’s a significant step towards the NHS’s vision of a single ‘front door’ for digital health.” Key Benefits for Patients and the NHS: ● One seamless journey: Patients and clinicians benefit from a more unified experience across apps and services. ● Better outcomes through joined-up care: Shared access to data empowers more personalised and timely interventions. ● Greater access to services: Patients can engage with support tools and resources anytime, anywhere. ● Reduced clinical workload: Digitally enhanced care pathways streamline processes and free up clinical time. ● Scalable long-term condition support: Proven tools for managing COPD, asthma, diabetes, and more, integrated with national systems. ● Patient empowerment: Enabling people to be active participants in their health journey. This partnership also honours the early vision of digital health pioneer Dr Warner Slack, who said in the 1970s: “I hoped that the computer would help the doctor in the care of the patient. And in the back of my mind was the idea that the computer might actually help patients to help themselves with their medical problems.” Today , that vision is becoming reality - placing digital tools directly in the hands of patients and enabling a more connected, compassionate, and sustainable NHS. About my mhealth my mhealth provides evidence-based digital therapeutics for patients with long-term conditions including COPD, asthma, diabetes, and heart disease. Trusted by NHS organisations across the UK, their platforms deliver scalable self-management support and remote monitoring tools that improve outcomes and reduce healthcare burden. About Patients Know Best Patients Know Best is the World’s largest Personal Health Record (PHR) and patient engagement platform, integrating data feeds from over 550 health organisations and providers. The system connects information from GPs, hospitals, social and mental health care providers, to create a single, unified copy of patient data. Everything from appointments and letters to test results, care plans, real-time monitoring data and discharge summaries, as well as the patient’s own data, are all available in one patient record, enabling patients and healthcare professionals to access up-to-date health information anytime, anywhere. In the UK, the platform serves over 5 million patients, registering 100,000+ patients and releasing over 20 million test results a month. PKB integrates with the NHS App to provide a single front door for patients to access their information.

NHS University College London Hospitals NHS Foundation Trust, part of North Central London ICB, is taking a significant step towards enhancing patient empowerment and optimising disease management. Asthma is a chronic condition that affects millions of people worldwide, often leading to severe health complications if not managed properly. Recognising the critical need for effective self-management tools, NHS University College London Hospitals NHS Foundation Trust has chosen the myAsthma app to provide patients with the resources they need to take control of their health. Dr Kay Roy PhD FRCP, Consultant Respiratory Physician University College London Hospitals NHS Foundation Trust, comments “We are thrilled to introduce myAsthma as a self-management tool to our community. It represents a significant step forward in empowering our patients with asthma to take control of their health. By providing them with personalised support, we believe this tool will greatly improve their quality of life. Additionally, the use of myAsthma in outpatient settings will help triage patients more effectively, ensuring they are seen in a timely manner and appropriately referred for the right investigations and services. Our team is excited to see the positive impact this will have on the asthma population across North Central London ICB." The myAsthma app, part of the my mhealth suite of digital health solutions, is designed to empower patients with comprehensive tools and information to manage their asthma more effectively. Key features include: • Personalised Action Plans: Tailored asthma management plans based on individual patient needs. • Inhaler technique training: Contributing to better health outcomes and reduced risk of exacerbations • Medication Tracking: Reminders and logs to ensure patients take their medication as prescribed. • Symptom tracking: Easy-to-use tools for tracking symptoms and triggers. • Educational Resources: Access to a wealth of information on asthma, helping patients understand their condition and how to manage it. As more NHS partners embrace the my mhealth platform, we're thrilled to witness its growing impact and the positive changes it is bringing to long-term condition care. For more information on this article or other my mhealth projects, please get in touch https://mymhealth.com/contact-us
Henry M.G. Glyde1Alison M. Blythin2 Tom M.A. Wilkinson3Ian T. Nabney4 James W. Dodd5 EPSRC Centre for Doctoral Training in Digital Health and Care, University of Bristol, Bristol, UK my mHealth Limited, Bournemouth , UK my mHealth and Clinical and Experimental Science, University of Southampton, Southampton, UK School of Engineering Mathematics and Technology, University of Bristol, Bristol, UK Academic Respiratory Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK Abstract Background Acute exacerbations of COPD (AECOPD) are episodes of breathlessness, cough and sputum which are associated with the risk of hospitalisation, progressive lung function decline and death. They are often missed or diagnosed late . Accurate timely intervention can improve these poor outcomes. Digital tools can be used to capture symptoms and other clinical data in COPD. This study aims to apply machine learning to the largest available real-world digital dataset to identify AECOPD Prediction tool which could be used to support early intervention improve clinical outcomes. Objective To create and validate a machine learning predictive model that forecasts exacerbations of COPD 1-8 days in advance. The model is based on routine patient-entered data from myCOPD self-management app. Method Adaptations of the AdaBoost algorithm were employed as machine learning approaches. The dataset included 506 patients users between 2017-2021. 55,066 app records were available for stable COPD event labels and 1,263 records of AECOPD event labels. The data used for training the model included COPD assessment test (CAT) scores, symptom scores, smoking history, and previous exacerbation frequency. All exacerbation records used in the model were confined to the 1-8 days preceding a self-reported exacerbation event. Results TheEasyEnsemble Classifier resulted in a Sensitivity of 67.0% and a Specificity of 65% with a positive predictive value (PPV) of 5.0% and a negative predictive value (NPV) of 98.9%. An AdaBoost model with a cost-sensitive decision tree resulted in a a Sensitivity of 35.0% and a Specificity of 89.0% with a PPV of 7.08% and NPV of 98.3%. Conclusion This preliminary analysis demonstrates that machine learning approaches to real-world data from a widely deployed digital therapeutic has the potential to predict AECOPD and can be used to confidently exclude the risk of exacerbations of COPD within the next 8 days. Permission to use received from Henry Glyde. Read more on Heliyon website.
Charlotte Smith 1 Francesca D’angelo 2 University Hospital of Derby and Burton, Cardiac Rehabilitation Department, Burton Upon Trent, UK. University Hospital of Derby and Burton, Health and Wellbeing Department, Burton, UK To examine the effectiveness of physical activity outcomes using a web-based Cardiac Rehabilitation application compared with a conventional programme or a combination of both. University Hospitals of Derby and Burton NHS Foundation Trust poster presented at the BACPR Annual Conference October 5-6th 2023 Permission to use received from Charlotte Smith
Francesca D’angelo 1 Charlotte Smith 2 University Hospital of Derby and Burton, Health and Wellbeing Department, Burton, UK University Hospital of Derby and Burton, Cardiac Rehabilitation Department, Burton Upon Trent, UK. To examine the effectiveness of psychological outcomes using a web-based Cardiac Rehabilitation application compared with a conventional programme or a combination of both. University Hospitals of Derby and Burton NHS Foundation Trust poster presented at the BACPR Annual Conference October 5-6th 2023 Poster presented at the BACPR Annual Conference October 5-6th 2023 Permission to use received from Charlotte Smith