How to achieve 2028 NHS England Long-Term Plan Targets for cardiac rehab
Dorset County Hospital NHS Foundation Trust Cardiac Rehabilitation team have hit the 2028 NHS targets for the past two years by adopting a new approach utilising the my mhealth app, myHeart.

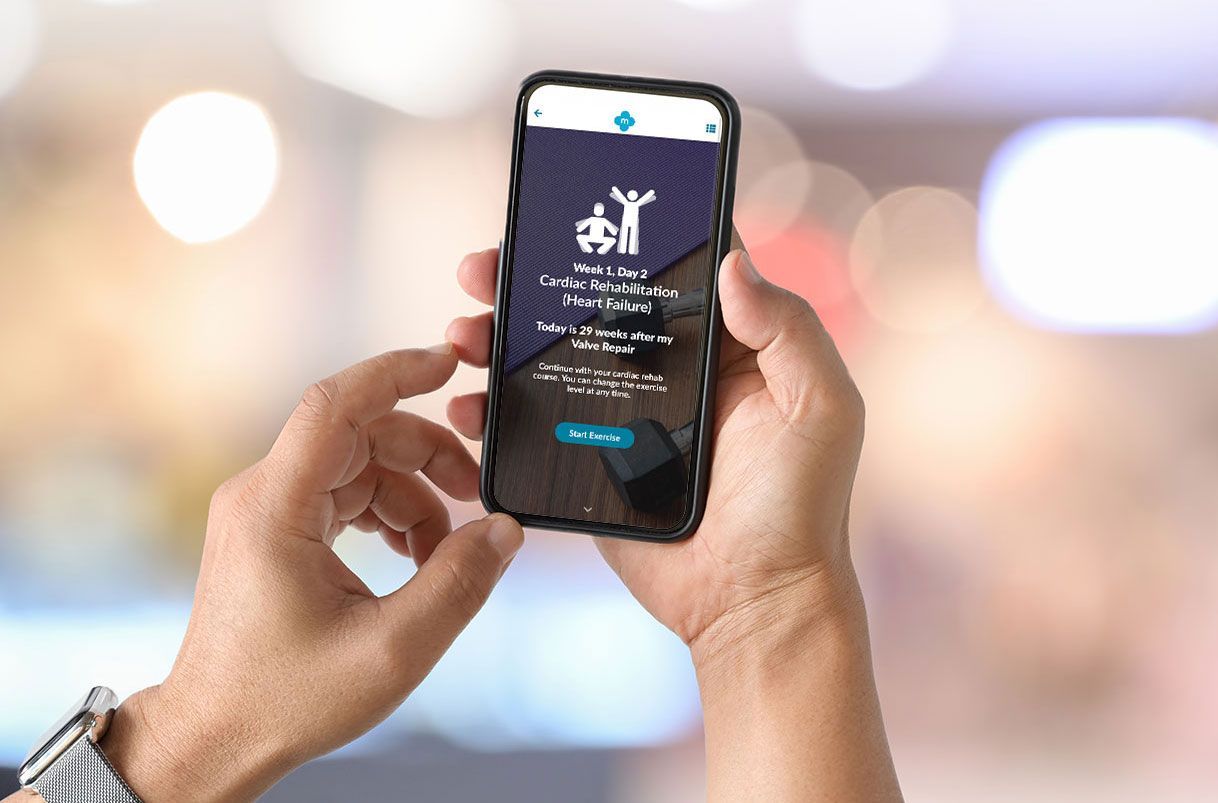
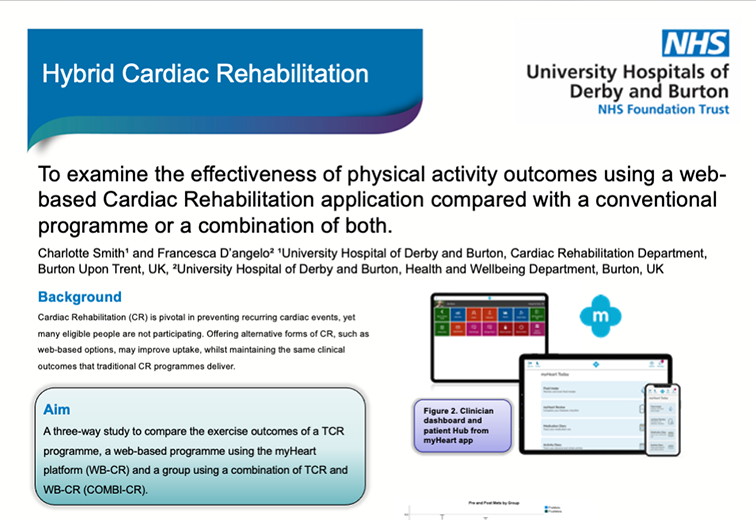
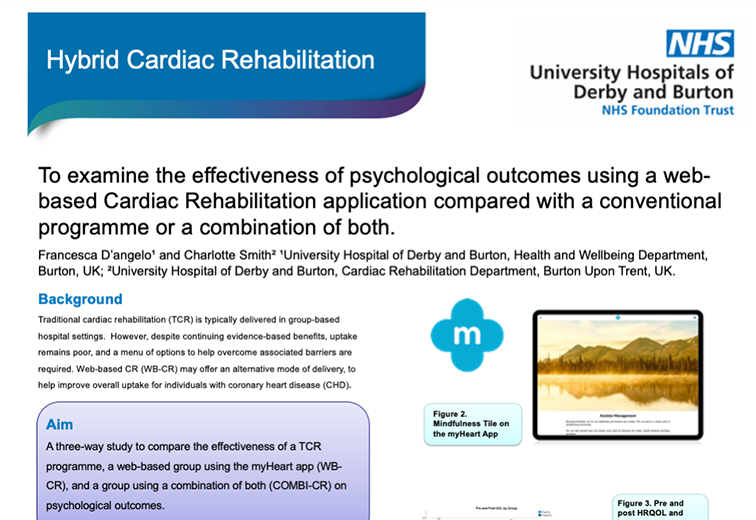
In 2017, the Dorset CR team and my mhealth developed an innovative CR module within myHeart to offer patients a digital component to compliment both traditional in-person and home-based models of CR delivery. The impact of utilising myHeart for CR uptake can be seen in the table below, with the services already exceeding the NHSE targets for 2028:
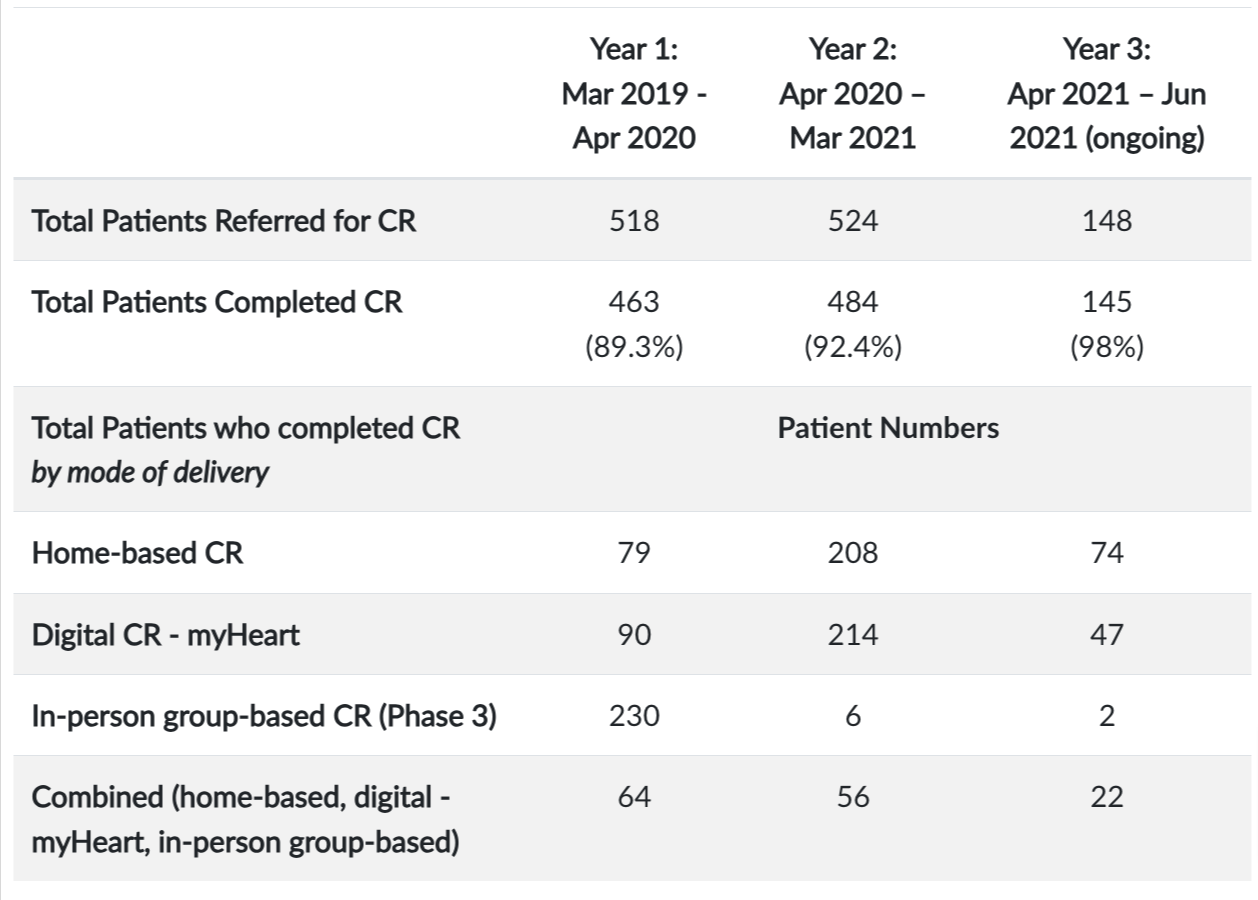
In March 2020, most traditional in-person CR programmes were suspended due to Covid-19. There was a rapid demand to quickly identify and adopt alternative ways of delivering CR to patients. However, the team in Dorset, due to the increased flexibility and resilience of their service model, simply suspended traditional in-person CR delivery and offered patients one of the other available options. myHeart usage increased by 124 (23.7%) patients during the first Covid-19 wave and continues to be a popular option for patients with a further 32.4% opting to use it in the first three months of year 3. These results show that digital health can contribute to supporting CR services to achieve greater patient uptake and completion rates.
Cardiac Rehab Specialist Nurse Shaun Porter told us...
"The menu-based approach of cardiac rehabilitation, has allowed us to provide an individually appropriate cardiac rehabilitation service to all of our patients, irrespective of physical conditions, ability to travel, IT literacy or socio-economic status. This, coupled with our holistic cardiac event follow-up clinic, ensures that all patients are assessed and treated promptly and holistically following their cardiac event."
The digitally enhanced approach adopted in Dorset has increased uptake to Cardiac Rehabilitation to consistently achieve and surpass the NHS targets for 2028 and increase service resilience.
"The myHeart App has proved really popular with patients and complements the other group-based and individual treatment options the rehab team offer. More cardiac patients than ever before are now receiving some form of rehab thanks to developments such as myHeart, which is having a hugely positive impact on people’s recovery and quality of life."
If you want to find out more about how digitally enhanced cardiac rehab can help you meet the NHS England Long-Term Targets for cardiac rehab please get in touch here or call us on +44 (0)1202 299 583.