my mhealth’s COVID-19 Virtual Ward app receives first patients from West Hampshire.
Dr Jessica Pickford knew that a digital solution was required to support her patients at scale, and not just with COVID-19.

Last week, Waterside PCN became the first PCN in the UK to go live with the my mhealth COVID-19 Virtual Ward app. Waterside PCN is a group of 5 surgeries based in West Hampshire, who have started digitally transforming their patient pathway, by providing their patients with access to our entire Long-Term Condition (LTC) platform. Patients suspected to have, or diagnosed with coronavirus, will now have access to the COVID-19 Virtual Ward alongside the other apps.
The COVID-19 Virtual Ward app uses a clinically recognised scoring algorithm to assist patients being managed in a virtual environment to be cared for remotely by their clinical team. By answering questions and recording a few measurements twice a day using a pulse oximeter, the patients provide their clinical team with the information needed to monitor their symptoms remotely.
The app has enabled us to monitor patients safely at home who we otherwise would have either needed to bring back daily for saturation monitoring or would have required admission.
The Waterside PCN team provided patients with access to a pulse oximeter, enabling them to accurately measure their oxygen levels and add their results to the Covid-19 virtual ward. We asked Dr Jessica Pickford, of the Red and Green Practice, to tell us how the app is helping her patients. She told us:
‘’The Waterside PCN has been itching to get going with the LTC apps since we discovered them towards the tail end of last year. The final trigger was the onset of the COVID-19 pandemic and the subsequent development of the COVID-19 Virtual Ward app. The combination of these apps provided an instant set of solutions to an acute and unprecedented set of complex problems not seen on this scale in primary care before.
With the nation in lockdown, how were we going to provide the same level of care and monitoring to our patients with LTCs? The very people who are deemed most vulnerable and in most need of regular health provision now find themselves in the position of being put at risk by just coming to the surgery. Of course, the other, more acutely worrying dilemma was how were we to effectively monitor those patients in the community with potential COVID-19 infection?
We know from the evidence coming out of China and Italy that people with COVID-19 can show quite mild symptoms one day and then be very unwell requiring hospitalisation within 48hours. One of the earliest signs of deterioration is a drop in their oxygen saturations which is often not associated, at least initially, with a worsening of symptoms. How were we going to keep patients at home that could be following this path? The solution came with the COVID-19 Virtual Ward app. Following remote telephone triage, the practices within the network can issue patients with potential COVID-19 symptoms pulse oximeter and a thermometer. These are then collected from the hot site by a family member or friend. This enables the patient to input their observations into the COVID-19 app and score their symptoms. Algorithms within the app then presents relevant alerts and advice to the patient and present this within a dashboard that can be visualised remotely from the hot hub.
The app has enabled us to monitor patients safely at home who we otherwise would have either needed to bring back to the hot hub daily for saturation monitoring or would have required admission. It also allows us to react quickly to those patients who are showing the early signs of deterioration but who would otherwise not seek help.
We have been able to utilise the long-term apps alongside the COVID-19 Virtual Ward app in several ways. Firstly, that people with diabetes are at increased risk of hyperglycaemia and Diabetes Ketoacidosis (DKA) with COVID-19. Combining the myDiabetes app with the COVID-19 Virtual Ward app assists the GP in monitoring people with diabetes who develop COVID-19 closely and again enables them to react quickly and admit the patient if needed.
Secondly, with regards to patients with Chronic Obstructive Pulmonary Disease (COPD) and asthma, it can be difficult to determine if their symptoms are just due to an exacerbation of their LTC or if it is the early signs of COVID-19. By combining the two apps we can safely monitor observations and symptoms for the potential of COVID-19 whilst assisting with the management of their LTC.
We have been very clear to patients that they are to not rely on the clinician monitoring the dashboard but should note the prompts generated by the apps and react accordingly. We promote the persons ’ownership’ of their LTC and the apps are a perfect platform for this. They are full of self-help videos, education and self-management opportunities. The dashboard gives the clinician a very quick and simple overview of the patient data within the individual apps enabling quick decisions and support.
Aside from COVID-19, the LTC apps provide us with a solution to the issue of maintaining LTC support and advice whilst working in a remote environment. Our patients have found the apps very simple to set up. Patients of all ages are utilising them with ease and are excited to use them. Our diabetes, asthma and COPD nurses can also benefit from having our patients use these apps. Not only do the apps assist with the accumulation of data remotely, but they also improve the patient's engagement, insight and management of their own health, and save us significant amounts of time trying to collate all the relevant information for the yearly reviews and QOF. The apps are revolutionising our way of working and improving our patient care.
If you're a healthcare professional or clinician and want to know more about how COVID-19 Virtual Ward can help your patients, you can find out more at www.mymhealth.com or by calling my mhealth on 0044 (0)1202 299 583
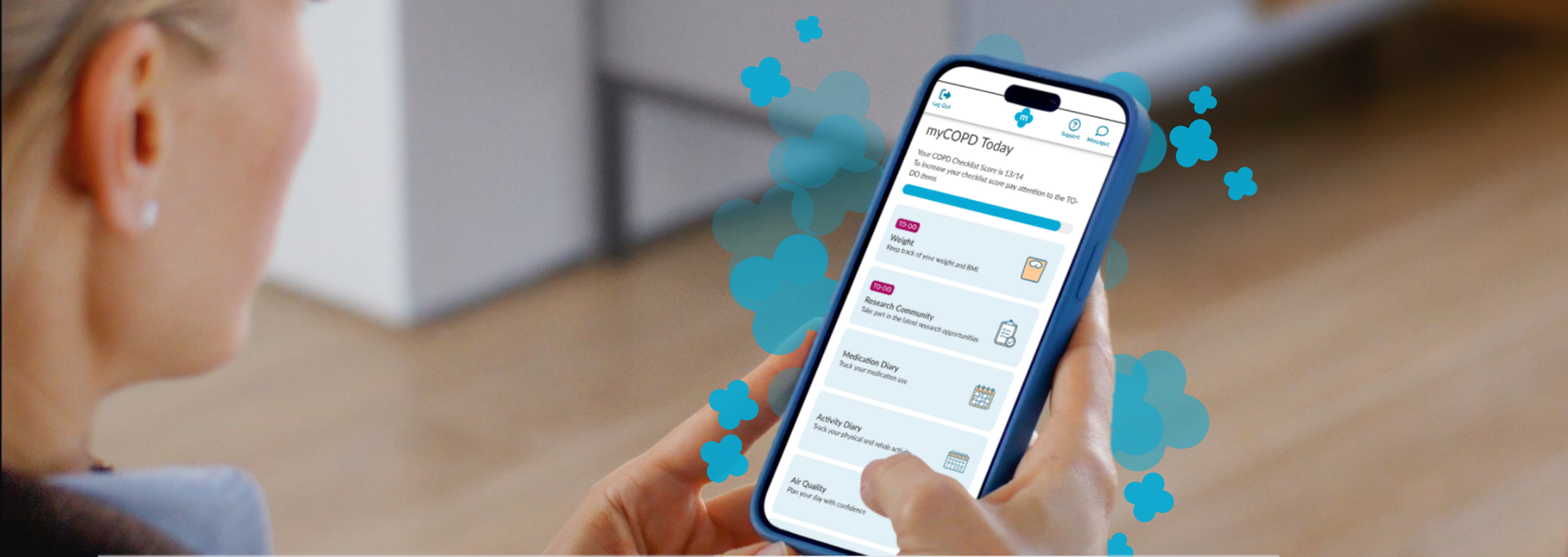
Your Feedback, Our Improvements We want to make sure our product is designed with your needs in mind. To achieve this, we regularly send out surveys and work closely with our Patient & Public Involvement (PPI) group, ensuring that your feedback directly shapes improvements and updates. We received 147 responses to our Research Community Survey .. said they found our app easy to use Overall, most of you said you had positive experiences of using the app .. said you would keep using it to manage your condition Our PPI activities have helped us to make important changes... Navigating around isn’t always that easy The home screen menu is now grouped into smaller sections with a ‘To Do’ list to help you stay on track Too many questions at the start makes it just too complicated Most of the questions at the start have now been removed so you can get started sooner We have now expanded the nutrition information which also contains a nutrition questionnaire to provide you with personalised advice There is not enough information on nutrition. Sometimes I forget to eat What we are working on We are creating a ‘Prepare for Your Appointment’ function in myCOPD and myAsthma We are planning to include a ‘Search’ function so you can get to what you need quickly Keep talking to us! Your experiences help us continue to improve.If you would like to share your thoughts or be part of our Patient and Public Involvement group, please join the Research Community. We would love to hear from you

A new partnership between leading digital health innovators, my mhealth and Patients Know Best (PKB) means shared NHS customers can streamline the delivery of their digital care tools, making it easier to empower patients to manage their health effectively. The collaboration brings together my mhealth’s award-winning self-management platforms with PKB’s personal health record solution, which is already embedded within the NHS App. “At the heart of this partnership is the patient,” said Dr. David Pettigrew, CEO of my mhealth . “By aligning our platforms, we’re enabling people to take greater control of their health while supporting clinicians with joined-up, efficient care pathways. It’s a significant step towards the NHS’s vision of a single ‘front door’ for digital health.” Key Benefits for Patients and the NHS: ● One seamless journey: Patients and clinicians benefit from a more unified experience across apps and services. ● Better outcomes through joined-up care: Shared access to data empowers more personalised and timely interventions. ● Greater access to services: Patients can engage with support tools and resources anytime, anywhere. ● Reduced clinical workload: Digitally enhanced care pathways streamline processes and free up clinical time. ● Scalable long-term condition support: Proven tools for managing COPD, asthma, diabetes, and more, integrated with national systems. ● Patient empowerment: Enabling people to be active participants in their health journey. This partnership also honours the early vision of digital health pioneer Dr Warner Slack, who said in the 1970s: “I hoped that the computer would help the doctor in the care of the patient. And in the back of my mind was the idea that the computer might actually help patients to help themselves with their medical problems.” Today , that vision is becoming reality - placing digital tools directly in the hands of patients and enabling a more connected, compassionate, and sustainable NHS. About my mhealth my mhealth provides evidence-based digital therapeutics for patients with long-term conditions including COPD, asthma, diabetes, and heart disease. Trusted by NHS organisations across the UK, their platforms deliver scalable self-management support and remote monitoring tools that improve outcomes and reduce healthcare burden. About Patients Know Best Patients Know Best is the World’s largest Personal Health Record (PHR) and patient engagement platform, integrating data feeds from over 550 health organisations and providers. The system connects information from GPs, hospitals, social and mental health care providers, to create a single, unified copy of patient data. Everything from appointments and letters to test results, care plans, real-time monitoring data and discharge summaries, as well as the patient’s own data, are all available in one patient record, enabling patients and healthcare professionals to access up-to-date health information anytime, anywhere. In the UK, the platform serves over 5 million patients, registering 100,000+ patients and releasing over 20 million test results a month. PKB integrates with the NHS App to provide a single front door for patients to access their information.

NHS University College London Hospitals NHS Foundation Trust, part of North Central London ICB, is taking a significant step towards enhancing patient empowerment and optimising disease management. Asthma is a chronic condition that affects millions of people worldwide, often leading to severe health complications if not managed properly. Recognising the critical need for effective self-management tools, NHS University College London Hospitals NHS Foundation Trust has chosen the myAsthma app to provide patients with the resources they need to take control of their health. Dr Kay Roy PhD FRCP, Consultant Respiratory Physician University College London Hospitals NHS Foundation Trust, comments “We are thrilled to introduce myAsthma as a self-management tool to our community. It represents a significant step forward in empowering our patients with asthma to take control of their health. By providing them with personalised support, we believe this tool will greatly improve their quality of life. Additionally, the use of myAsthma in outpatient settings will help triage patients more effectively, ensuring they are seen in a timely manner and appropriately referred for the right investigations and services. Our team is excited to see the positive impact this will have on the asthma population across North Central London ICB." The myAsthma app, part of the my mhealth suite of digital health solutions, is designed to empower patients with comprehensive tools and information to manage their asthma more effectively. Key features include: • Personalised Action Plans: Tailored asthma management plans based on individual patient needs. • Inhaler technique training: Contributing to better health outcomes and reduced risk of exacerbations • Medication Tracking: Reminders and logs to ensure patients take their medication as prescribed. • Symptom tracking: Easy-to-use tools for tracking symptoms and triggers. • Educational Resources: Access to a wealth of information on asthma, helping patients understand their condition and how to manage it. As more NHS partners embrace the my mhealth platform, we're thrilled to witness its growing impact and the positive changes it is bringing to long-term condition care. For more information on this article or other my mhealth projects, please get in touch https://mymhealth.com/contact-us
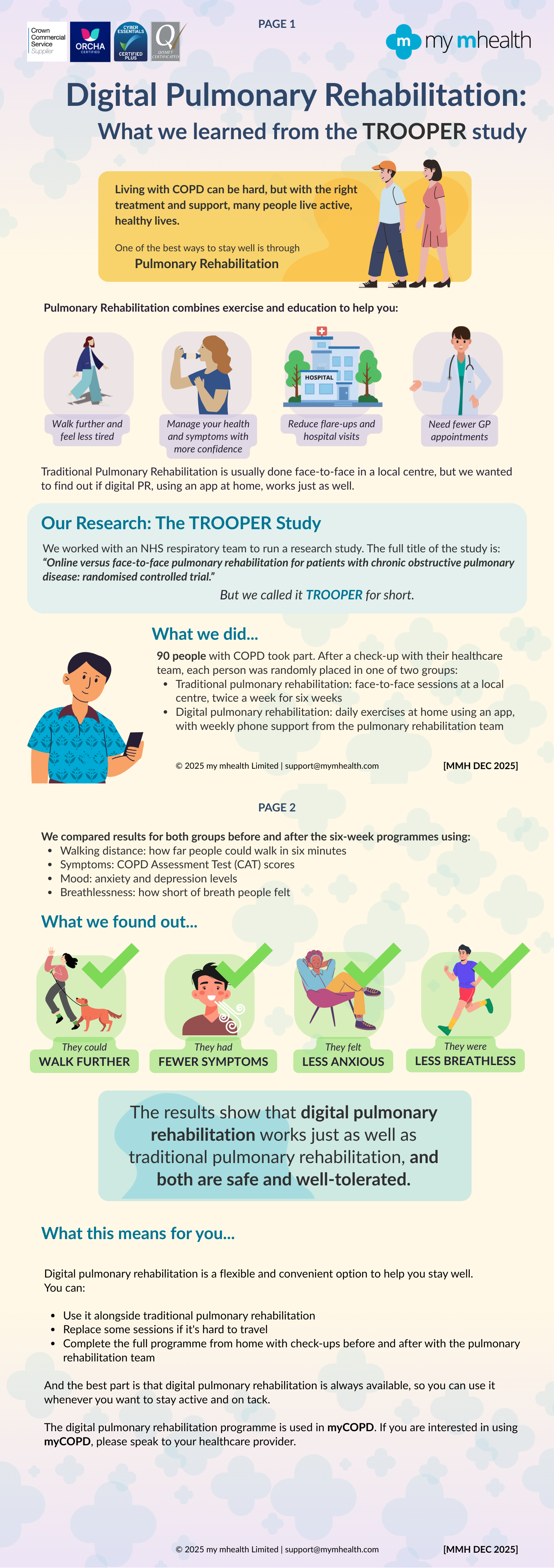
Henry M.G. Glyde1Alison M. Blythin2 Tom M.A. Wilkinson3Ian T. Nabney4 James W. Dodd5 EPSRC Centre for Doctoral Training in Digital Health and Care, University of Bristol, Bristol, UK my mHealth Limited, Bournemouth , UK my mHealth and Clinical and Experimental Science, University of Southampton, Southampton, UK School of Engineering Mathematics and Technology, University of Bristol, Bristol, UK Academic Respiratory Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK Abstract Background Acute exacerbations of COPD (AECOPD) are episodes of breathlessness, cough and sputum which are associated with the risk of hospitalisation, progressive lung function decline and death. They are often missed or diagnosed late . Accurate timely intervention can improve these poor outcomes. Digital tools can be used to capture symptoms and other clinical data in COPD. This study aims to apply machine learning to the largest available real-world digital dataset to identify AECOPD Prediction tool which could be used to support early intervention improve clinical outcomes. Objective To create and validate a machine learning predictive model that forecasts exacerbations of COPD 1-8 days in advance. The model is based on routine patient-entered data from myCOPD self-management app. Method Adaptations of the AdaBoost algorithm were employed as machine learning approaches. The dataset included 506 patients users between 2017-2021. 55,066 app records were available for stable COPD event labels and 1,263 records of AECOPD event labels. The data used for training the model included COPD assessment test (CAT) scores, symptom scores, smoking history, and previous exacerbation frequency. All exacerbation records used in the model were confined to the 1-8 days preceding a self-reported exacerbation event. Results TheEasyEnsemble Classifier resulted in a Sensitivity of 67.0% and a Specificity of 65% with a positive predictive value (PPV) of 5.0% and a negative predictive value (NPV) of 98.9%. An AdaBoost model with a cost-sensitive decision tree resulted in a a Sensitivity of 35.0% and a Specificity of 89.0% with a PPV of 7.08% and NPV of 98.3%. Conclusion This preliminary analysis demonstrates that machine learning approaches to real-world data from a widely deployed digital therapeutic has the potential to predict AECOPD and can be used to confidently exclude the risk of exacerbations of COPD within the next 8 days. Permission to use received from Henry Glyde. Read more on Heliyon website.
Charlotte Smith 1 Francesca D’angelo 2 University Hospital of Derby and Burton, Cardiac Rehabilitation Department, Burton Upon Trent, UK. University Hospital of Derby and Burton, Health and Wellbeing Department, Burton, UK To examine the effectiveness of physical activity outcomes using a web-based Cardiac Rehabilitation application compared with a conventional programme or a combination of both. University Hospitals of Derby and Burton NHS Foundation Trust poster presented at the BACPR Annual Conference October 5-6th 2023 Permission to use received from Charlotte Smith
Francesca D’angelo 1 Charlotte Smith 2 University Hospital of Derby and Burton, Health and Wellbeing Department, Burton, UK University Hospital of Derby and Burton, Cardiac Rehabilitation Department, Burton Upon Trent, UK. To examine the effectiveness of psychological outcomes using a web-based Cardiac Rehabilitation application compared with a conventional programme or a combination of both. University Hospitals of Derby and Burton NHS Foundation Trust poster presented at the BACPR Annual Conference October 5-6th 2023 Poster presented at the BACPR Annual Conference October 5-6th 2023 Permission to use received from Charlotte Smith