Digital therapy for anxiety using mindfulness treatments in virtual reality (VR).
How my mhealth, Bournemouth University and Innovate UK joined forces to tackle mental health with a VR app.

At my mhealth we strive to improve the health and quality of life of people and see technological innovation as an exciting vehicle to achieve this. Our teams of doctors and technologists are constantly looking for new treatments and technologies to help meet our ambitions, be it self-management, education, rehabilitation, interventions or therapeutics. And not just for the few, we want to do this at scale, so everyone gets the chance to benefit
This is what my mhealth is all about.
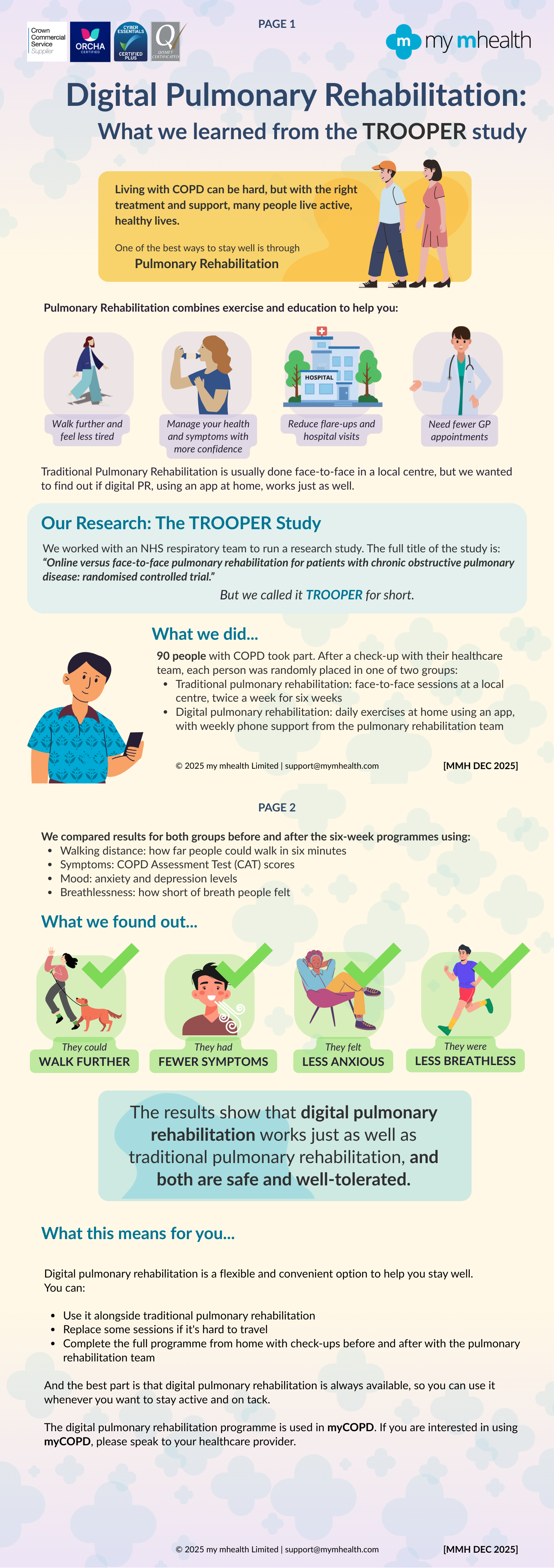
We've done it for COPD, we've done it for asthma, diabetes and heart disease. And now we've done it for mental health.
The prevalence of anxiety disorders across the world varies from 2.5 to 7 per cent by country. Globally an estimated 284 million people experienced an anxiety disorder in 2017, making it the most prevalent mental health or neurodevelopmental disorder (1).
Mental health is without a doubt an illness that can be significantly improved using digital therapeutics such as virtual reality, and global investment in digital therapeutics is higher for psychiatry than any other type of illness.
That's why in 2019 we invested in a study to understand the effectiveness of virtual reality therapy for anxiety-related mental health conditions. In a collaborative partnership with Bournemouth University and Innovate UK, Robert Farthing, our VR developer, has built a digital therapy using immersive VR as a treatment for anxiety.
Rob Farthing, the principal developer told us:
"Over the past few months, there has been much discussion of mental health, so this project feels more relevant than ever, having the potential to help people who are isolated through creating a means of teaching mindfulness to manage stress and anxiety digitally. During the lock-down, we are seeing increases in adoption of technology to stay connected; there are also ongoing studies into how VR in particular is helping to address the psychological effects of global quarantines through travelling to relaxing virtual locations."
The digital therapy treats patients using existing cognitive behavioural therapy (CBT) and mindful meditation techniques and is designed to complement rather than fully replace traditional therapy delivered by a therapist.
The VR mindfulness app enables people to focus on relaxation techniques without the distractions of the outside world. The immersion offered by virtual reality gives people a sense of 'presence' in a 3D computer-generated world, helping them to practice mindfulness in a controlled manner.
Handheld controllers connected to the VR headset, or the headset itself, track the user's motions during exercise, meditation and breathing exercises and patients can see a representation of themselves in the world we've created. Patients can even go as far as interacting with the landscape. For example, picking up a flower and focusing on the petals, changing the colour of their petals one by one. Or strolling through the virtual landscapes.
We're very excited to see the outcomes of the first real-world trials and to develop the VR software further. With the cost of VR headsets falling, and VR technology advancing rapidly, the cost and speed of delivering this type of therapy via VR will be more efficient than traditional methods. We envisage that therapists will loan patients the VR headsets with our software pre-loaded to complete their treatment in the comfort of their own homes.
1. Mental Health by Hannah Ritchie and Max Roser, 2018.
If you'd like to find out more about digital therapeutics or want to know more about how we can help you or your patients get in touch here or call us on 0044 (0)1202 299 583.
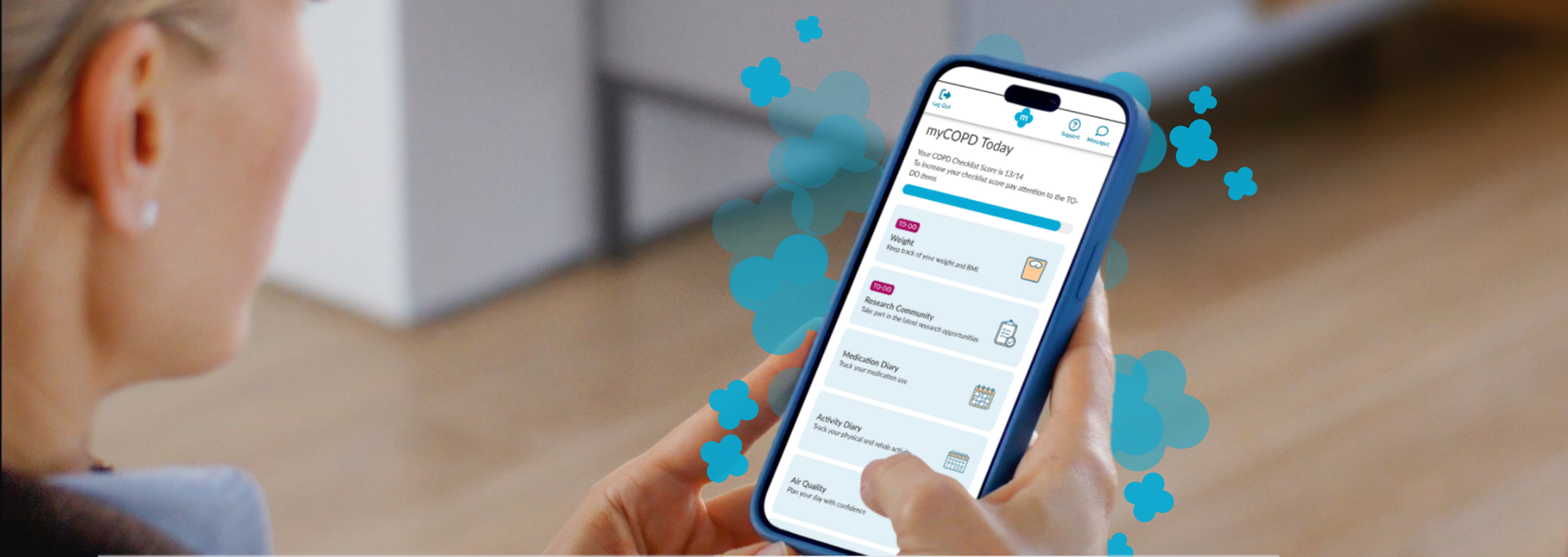
Your Feedback, Our Improvements We want to make sure our product is designed with your needs in mind. To achieve this, we regularly send out surveys and work closely with our Patient & Public Involvement (PPI) group, ensuring that your feedback directly shapes improvements and updates. We received 147 responses to our Research Community Survey .. said they found our app easy to use Overall, most of you said you had positive experiences of using the app .. said you would keep using it to manage your condition Our PPI activities have helped us to make important changes... Navigating around isn’t always that easy The home screen menu is now grouped into smaller sections with a ‘To Do’ list to help you stay on track Too many questions at the start makes it just too complicated Most of the questions at the start have now been removed so you can get started sooner We have now expanded the nutrition information which also contains a nutrition questionnaire to provide you with personalised advice There is not enough information on nutrition. Sometimes I forget to eat What we are working on We are creating a ‘Prepare for Your Appointment’ function in myCOPD and myAsthma We are planning to include a ‘Search’ function so you can get to what you need quickly Keep talking to us! Your experiences help us continue to improve.If you would like to share your thoughts or be part of our Patient and Public Involvement group, please join the Research Community. We would love to hear from you

A new partnership between leading digital health innovators, my mhealth and Patients Know Best (PKB) means shared NHS customers can streamline the delivery of their digital care tools, making it easier to empower patients to manage their health effectively. The collaboration brings together my mhealth’s award-winning self-management platforms with PKB’s personal health record solution, which is already embedded within the NHS App. “At the heart of this partnership is the patient,” said Dr. David Pettigrew, CEO of my mhealth . “By aligning our platforms, we’re enabling people to take greater control of their health while supporting clinicians with joined-up, efficient care pathways. It’s a significant step towards the NHS’s vision of a single ‘front door’ for digital health.” Key Benefits for Patients and the NHS: ● One seamless journey: Patients and clinicians benefit from a more unified experience across apps and services. ● Better outcomes through joined-up care: Shared access to data empowers more personalised and timely interventions. ● Greater access to services: Patients can engage with support tools and resources anytime, anywhere. ● Reduced clinical workload: Digitally enhanced care pathways streamline processes and free up clinical time. ● Scalable long-term condition support: Proven tools for managing COPD, asthma, diabetes, and more, integrated with national systems. ● Patient empowerment: Enabling people to be active participants in their health journey. This partnership also honours the early vision of digital health pioneer Dr Warner Slack, who said in the 1970s: “I hoped that the computer would help the doctor in the care of the patient. And in the back of my mind was the idea that the computer might actually help patients to help themselves with their medical problems.” Today , that vision is becoming reality - placing digital tools directly in the hands of patients and enabling a more connected, compassionate, and sustainable NHS. About my mhealth my mhealth provides evidence-based digital therapeutics for patients with long-term conditions including COPD, asthma, diabetes, and heart disease. Trusted by NHS organisations across the UK, their platforms deliver scalable self-management support and remote monitoring tools that improve outcomes and reduce healthcare burden. About Patients Know Best Patients Know Best is the World’s largest Personal Health Record (PHR) and patient engagement platform, integrating data feeds from over 550 health organisations and providers. The system connects information from GPs, hospitals, social and mental health care providers, to create a single, unified copy of patient data. Everything from appointments and letters to test results, care plans, real-time monitoring data and discharge summaries, as well as the patient’s own data, are all available in one patient record, enabling patients and healthcare professionals to access up-to-date health information anytime, anywhere. In the UK, the platform serves over 5 million patients, registering 100,000+ patients and releasing over 20 million test results a month. PKB integrates with the NHS App to provide a single front door for patients to access their information.

NHS University College London Hospitals NHS Foundation Trust, part of North Central London ICB, is taking a significant step towards enhancing patient empowerment and optimising disease management. Asthma is a chronic condition that affects millions of people worldwide, often leading to severe health complications if not managed properly. Recognising the critical need for effective self-management tools, NHS University College London Hospitals NHS Foundation Trust has chosen the myAsthma app to provide patients with the resources they need to take control of their health. Dr Kay Roy PhD FRCP, Consultant Respiratory Physician University College London Hospitals NHS Foundation Trust, comments “We are thrilled to introduce myAsthma as a self-management tool to our community. It represents a significant step forward in empowering our patients with asthma to take control of their health. By providing them with personalised support, we believe this tool will greatly improve their quality of life. Additionally, the use of myAsthma in outpatient settings will help triage patients more effectively, ensuring they are seen in a timely manner and appropriately referred for the right investigations and services. Our team is excited to see the positive impact this will have on the asthma population across North Central London ICB." The myAsthma app, part of the my mhealth suite of digital health solutions, is designed to empower patients with comprehensive tools and information to manage their asthma more effectively. Key features include: • Personalised Action Plans: Tailored asthma management plans based on individual patient needs. • Inhaler technique training: Contributing to better health outcomes and reduced risk of exacerbations • Medication Tracking: Reminders and logs to ensure patients take their medication as prescribed. • Symptom tracking: Easy-to-use tools for tracking symptoms and triggers. • Educational Resources: Access to a wealth of information on asthma, helping patients understand their condition and how to manage it. As more NHS partners embrace the my mhealth platform, we're thrilled to witness its growing impact and the positive changes it is bringing to long-term condition care. For more information on this article or other my mhealth projects, please get in touch https://mymhealth.com/contact-us
Henry M.G. Glyde1Alison M. Blythin2 Tom M.A. Wilkinson3Ian T. Nabney4 James W. Dodd5 EPSRC Centre for Doctoral Training in Digital Health and Care, University of Bristol, Bristol, UK my mHealth Limited, Bournemouth , UK my mHealth and Clinical and Experimental Science, University of Southampton, Southampton, UK School of Engineering Mathematics and Technology, University of Bristol, Bristol, UK Academic Respiratory Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK Abstract Background Acute exacerbations of COPD (AECOPD) are episodes of breathlessness, cough and sputum which are associated with the risk of hospitalisation, progressive lung function decline and death. They are often missed or diagnosed late . Accurate timely intervention can improve these poor outcomes. Digital tools can be used to capture symptoms and other clinical data in COPD. This study aims to apply machine learning to the largest available real-world digital dataset to identify AECOPD Prediction tool which could be used to support early intervention improve clinical outcomes. Objective To create and validate a machine learning predictive model that forecasts exacerbations of COPD 1-8 days in advance. The model is based on routine patient-entered data from myCOPD self-management app. Method Adaptations of the AdaBoost algorithm were employed as machine learning approaches. The dataset included 506 patients users between 2017-2021. 55,066 app records were available for stable COPD event labels and 1,263 records of AECOPD event labels. The data used for training the model included COPD assessment test (CAT) scores, symptom scores, smoking history, and previous exacerbation frequency. All exacerbation records used in the model were confined to the 1-8 days preceding a self-reported exacerbation event. Results TheEasyEnsemble Classifier resulted in a Sensitivity of 67.0% and a Specificity of 65% with a positive predictive value (PPV) of 5.0% and a negative predictive value (NPV) of 98.9%. An AdaBoost model with a cost-sensitive decision tree resulted in a a Sensitivity of 35.0% and a Specificity of 89.0% with a PPV of 7.08% and NPV of 98.3%. Conclusion This preliminary analysis demonstrates that machine learning approaches to real-world data from a widely deployed digital therapeutic has the potential to predict AECOPD and can be used to confidently exclude the risk of exacerbations of COPD within the next 8 days. Permission to use received from Henry Glyde. Read more on Heliyon website.
Charlotte Smith 1 Francesca D’angelo 2 University Hospital of Derby and Burton, Cardiac Rehabilitation Department, Burton Upon Trent, UK. University Hospital of Derby and Burton, Health and Wellbeing Department, Burton, UK To examine the effectiveness of physical activity outcomes using a web-based Cardiac Rehabilitation application compared with a conventional programme or a combination of both. University Hospitals of Derby and Burton NHS Foundation Trust poster presented at the BACPR Annual Conference October 5-6th 2023 Permission to use received from Charlotte Smith
Francesca D’angelo 1 Charlotte Smith 2 University Hospital of Derby and Burton, Health and Wellbeing Department, Burton, UK University Hospital of Derby and Burton, Cardiac Rehabilitation Department, Burton Upon Trent, UK. To examine the effectiveness of psychological outcomes using a web-based Cardiac Rehabilitation application compared with a conventional programme or a combination of both. University Hospitals of Derby and Burton NHS Foundation Trust poster presented at the BACPR Annual Conference October 5-6th 2023 Poster presented at the BACPR Annual Conference October 5-6th 2023 Permission to use received from Charlotte Smith